HIPAA Compliant Push Notifications: A Complete Guide


Introduction: The Power of Secure Patient Engagement
In today’s digital-first world, the smartphone has become the central hub of our lives. We manage our finances, order groceries, connect with friends, and navigate our cities—all from the palm of our hand. This fundamental shift in behavior has permanently altered consumer expectations, and healthcare is no exception. The days of relying solely on mailed appointment cards and time-consuming phone tag are fading. Modern patients expect the same level of convenience, immediacy, and personalization from their healthcare providers that they receive from every other service. This is the new reality of patient communication, and at its forefront is the powerful, direct channel of mobile technology.
Harnessing this technology is no longer an option; it’s an imperative for providers who want to improve patient outcomes and operational efficiency. Among the tools available, push notifications have emerged as a uniquely effective solution. These short, direct messages sent from an application to a user’s mobile device are designed to deliver timely, relevant information that cuts through the noise of a crowded email inbox. When applied thoughtfully in a healthcare context, their benefits are transformative.
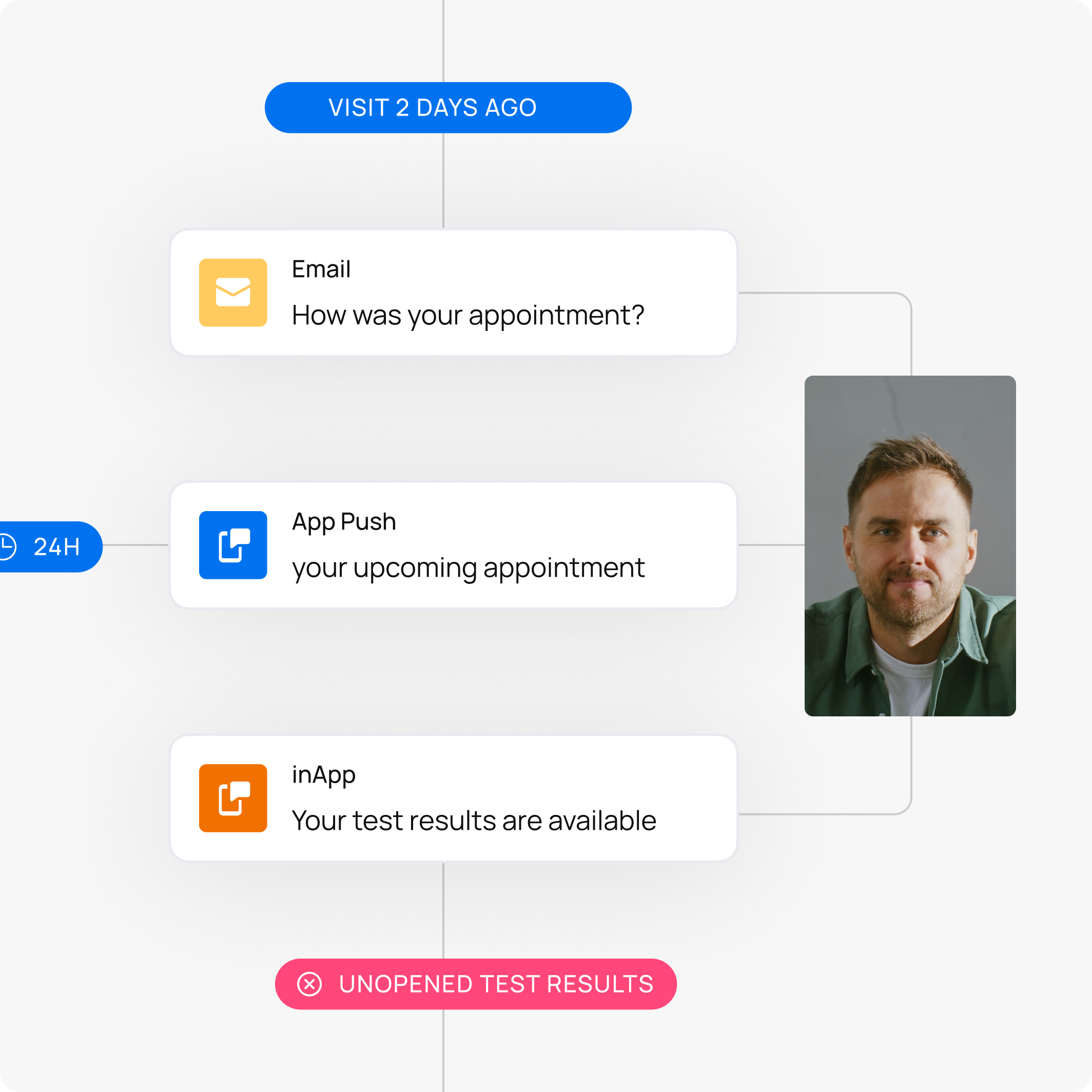
Consider the persistent challenge of patient no-shows, a problem that costs the U.S. healthcare system an estimated $150 billion annually. A simple, automated push notification sent 24 hours before an appointment serves as a powerful, just-in-time reminder that is far more likely to be seen than an email sent a week prior. This small action can dramatically reduce missed appointments, optimizing clinic schedules and ensuring continuity of care.
Beyond logistics, push notifications play a critical role in one of the most significant determinants of health outcomes: medication adherence. It’s estimated that non-adherence to prescribed medication causes approximately 125,000 deaths and at least 10% of hospitalizations each year. A discreet, personalized push notification can act as a private digital health assistant, gently reminding a patient to take their medication, request a refill, or follow post-operative care instructions. This continuous, supportive engagement helps bridge the gap between clinical visits, empowering patients to take a more active role in managing their own health. The result is better adherence, fewer complications, and healthier patients.
However, unlike a notification from a retail app announcing a sale, healthcare communication carries an immense weight of responsibility. Every message, no matter how brief, exists within the stringent regulatory framework of the Health Insurance Portability and Accountability Act (HIPAA). Sending an appointment reminder or a message about test results involves Protected Health Information (PHI), and the unauthorized disclosure of this data can lead to severe financial penalties and, more importantly, an irreversible erosion of patient trust. This creates a critical dilemma for healthcare organizations: How can you leverage the immense power of push notifications to engage patients without exposing your organization and your patients to risk?
This is the central challenge that we solve. As a leader in omnichannel digital communication, indigitall understands this critical balance between effective engagement and ironclad security. Our mission is to empower healthcare providers to build meaningful, lasting relationships with their patients through secure, reliable, and compliant technology. We believe you shouldn’t have to choose between innovation and security. This guide shares our deep expertise on navigating the complexities of HIPAA, providing you with a clear roadmap to implementing a push notification strategy that is not only powerful but, above all, safe.
What is HIPAA and Why it Applies to Your Push Notifications
To build a secure patient communication strategy, it’s essential to first understand the framework that governs it. The Health Insurance Portability and Accountability Act of 1996 (HIPAA) is often viewed as a complex set of restrictive rules, but its core purpose is simple and noble: to protect the sanctity of a patient’s sensitive health information while allowing for the flow of that information to provide high-quality care. While enacted long before the first smartphone, HIPAA’s principles are technology-neutral, making them just as relevant to a 2025 push notification as they were to a 1996 paper file. Any communication channel that creates, receives, maintains, or transmits patient data falls squarely under its jurisdiction. Understanding how HIPAA applies requires looking at its three primary pillars.
Understanding the Three Pillars of HIPAA
HIPAA is not a single, monolithic rule but a composite of several key regulations. For digital communications like push notifications, three are most critical: the Privacy Rule, the Security Rule, and the Breach Notification Rule.
- The Privacy Rule: Governing What You Can Say The HIPAA Privacy Rule establishes national standards for the protection of Protected Health Information (PHI). It governs the circumstances under which a healthcare provider or business associate can use or disclose this sensitive data. In essence, it’s the “what” and “who” of patient data. For push notifications, the Privacy Rule dictates that you must have a patient’s explicit consent (an opt-in) to communicate with them via this channel for anything other than basic treatment and payment operations. It ensures that patients have control over their data and that it is not shared without their permission. Sending a notification with specific medical advice or health information without a proper consent framework is a direct violation of this rule.
- The Security Rule: Governing How You Send It While the Privacy Rule sets the guidelines for data use, the Security Rule dictates the technological and procedural safeguards required to protect it. This rule applies specifically to electronic PHI (ePHI) and is arguably the most critical component for your push notification strategy. It mandates three types of safeguards:
- Technical Safeguards: This includes the technology used to protect ePHI. For push notifications, the absolute cornerstone is end-to-end encryption (E2EE), which ensures data is unreadable to anyone except the intended recipient. It also includes access controls (ensuring only authorized staff can send messages) and audit controls (logging who accessed data and when).
- Administrative Safeguards: These are the policies and procedures that direct your team’s conduct. It involves risk analysis, staff training on security protocols, and, crucially, signing a Business Associate Agreement (BAA) with your notification vendor.
- Physical Safeguards: This covers the physical protection of systems and servers where ePHI is stored. Your vendor must demonstrate that their data centers are secure against physical intrusion and environmental hazards.
- The Breach Notification Rule: Your Plan for If Things Go Wrong No system is infallible. The Breach Notification Rule requires covered entities and their business associates to provide notification following a breach of unsecured PHI. Should your push notification platform be compromised, leading to unauthorized access to patient data, this rule outlines your legal obligation to notify the affected individuals, the Secretary of Health and Human Services, and in some cases, the media. Having a compliant partner and a clear incident response plan is essential to meeting these strict reporting deadlines and mitigating damage.
What is Protected Health Information (PHI) in a Push Notification?
The trigger for all these rules is the presence of PHI. Officially, PHI is any individually identifiable health information that relates to the past, present, or future physical or mental health of an individual. This includes at least one of the 18 HIPAA identifiers (like a name, date, or phone number) combined with a health-related data point.
In a push notification, PHI can be obvious and explicit. For example:
- “Reminder: Your annual physical with Dr. Evans is on October 15, 2025.”
- “Your prescription for Atorvastatin is ready for pickup at our pharmacy.”
- “A new lab result is available for you to view in the patient portal.”
However, the most overlooked risk is contextual PHI. The very act of sending a message from a specifically named provider to a patient’s device can be a disclosure of PHI, even if the message content is generic. Consider the difference:
- A notification from “City General Hospital” that says “You have a new message.” is low-risk.
- A notification from “The City Oncology & Hematology Center” that says “You have a new message.” is a serious potential breach. The name of the sender alone reveals a highly sensitive health condition, confirming that the recipient is a patient of that specialty clinic.
Think of it like an envelope. A plain, unmarked envelope delivered to a home is private. But an envelope with the return address of a renowned cancer treatment center reveals a great deal of information before it’s ever opened. A push notification is the digital version of that envelope, and its “from” field is just as important as its content. This is why a truly HIPAA-compliant solution must secure not only the message itself but also the metadata and the relationship between sender and receiver.
The High Stakes of Non-Compliance
Implementing a push notification strategy without a deep understanding of HIPAA is like navigating a minefield blindfolded. The potential for missteps is enormous, and the consequences are not just hypothetical—they are financially crippling and reputationally devastating. The Department of Health and Human Services (HHS) does not take the mishandling of Protected Health Information (PHI) lightly. For any healthcare organization, understanding the severe penalties for non-compliance is the first step toward appreciating the absolute necessity of a security-first approach to patient communication.
Financial Penalties and Reputational Damage
The financial penalties for HIPAA violations are structured in a tiered system based on the level of culpability, meaning the fines increase dramatically depending on whether the violation was accidental or due to willful neglect.
- Tier 1: Lack of Knowledge. This applies when a healthcare entity was unaware of the violation and could not have realistically avoided it, even with reasonable due diligence. Fines range from $137 to $68,928 per violation, with an annual cap of over $2 million. A hypothetical example could be a newly discovered software bug in a vendor’s platform that briefly exposed data despite the provider’s best efforts.
- Tier 2: Reasonable Cause. This tier covers violations where the entity knew or should have known about the rule through reasonable diligence but did not act with willful neglect. Fines range from $1,379 to $68,928 per violation, with the same annual cap. This might involve an organization failing to provide adequate HIPAA training to a new marketing employee who then sends an insecure push notification campaign.
- Tier 3: Willful Neglect, Corrected. Here, the violation was a result of intentional failure or conscious indifference to HIPAA rules, but the organization made efforts to correct the issue within 30 days. The penalties increase significantly, ranging from $13,785 to $68,928 per violation. An example would be knowingly using a non-compliant vendor but immediately terminating the contract and self-reporting after an internal audit discovered the risk.
- Tier 4: Willful Neglect, Not Corrected. This is the most severe category. The violation was intentional, and no meaningful effort was made to correct it in a timely manner. The fines are catastrophic, starting at a minimum of $68,928 per violation and reaching an annual maximum of $2,067,813. Continuing to use a cheap, non-compliant push notification provider after being warned of the risks by your IT team would fall squarely into this tier.
While these fines are staggering, the long-term damage to your organization’s reputation can be even more costly. A financial penalty is a one-time event; a loss of patient trust is a chronic condition. In an age of instant information, news of a data breach appears on social media and news outlets within hours, permanently associating your brand with insecurity. This breach will be publicly listed on the HHS “Wall of Shame,” creating a permanent digital record of the failure. Current patients may leave for providers they feel will better protect their sensitive data, and prospective patients will be wary of choosing you. The cost of marketing, public relations, and patient re-acquisition to repair this damage will almost certainly dwarf the initial government fine.
Common Pitfalls to Avoid
Fortunately, avoiding these consequences is possible by steering clear of common, yet critical, mistakes. These pitfalls represent the most frequent sources of HIPAA violations in digital communications.
- Sending PHI in Unencrypted Messages. Encryption is the bedrock of the HIPAA Security Rule. It scrambles data into an unreadable code that can only be unlocked with a specific key. Sending a push notification containing PHI without end-to-end encryption is the digital equivalent of mailing a patient’s diagnosis on a postcard for the world to see. It leaves the data vulnerable as it travels from your server to the patient’s device and can even expose it on the device’s lock screen. It is a direct and unambiguous violation.
- Partnering with a Vendor That Won’t Sign a BAA. A Business Associate Agreement (BAA) is a legally binding contract that obligates your technology vendor (the “business associate”) to protect PHI with the same rigor that you do. Without a signed BAA, the full legal liability for a breach caused by your vendor rests on your shoulders. A vendor’s refusal to sign a BAA is the single biggest red flag you can encounter. It signals they are not equipped or willing to handle sensitive health data, and partnering with them amounts to willful neglect.
- Lacking Proper Access Controls and Audit Logs. Not everyone on your staff needs the ability to send communications to every patient. Access controls ensure that employees only have access to the data and tools essential for their specific job (the principle of “least privilege”). This prevents accidental data exposure and internal misuse. Audit logs are the indispensable digital record of every action taken within the platform—who logged in, what they did, and when they did it. In the event of an incident, these logs are your only way to investigate what happened, demonstrate due diligence to regulators, and understand the scope of the breach. Operating without them is not only non-compliant but also dangerously shortsighted.

How indigitall Enables HIPAA Compliant Push Notifications
Understanding the rules of HIPAA is one thing; implementing them in practice requires a technology partner that has built security and compliance into the very fabric of its platform. At indigitall, compliance isn’t an afterthought or a feature—it’s the foundation upon which our entire communication ecosystem is built. We provide healthcare organizations with the tools to engage patients effectively, backed by a multi-layered security strategy that directly addresses the core requirements of the HIPAA Security Rule. Here is how we turn compliance theory into a secure reality.
End-to-End Encryption (E2EE) by Default
The most fundamental requirement for protecting electronic Protected Health Information (ePHI) is ensuring it remains confidential and unreadable to unauthorized parties. Indigitall achieves this through a mandatory, always-on, end-to-end encryption protocol for all communications containing sensitive data. Think of E2EE as sealing a critical message in a digital vault before it ever leaves our platform. This vault can only be unlocked by a unique key held by the intended recipient’s device, making the content completely unintelligible to anyone else.
This protection is comprehensive, covering data at every stage of its journey:
- Data in Transit: As a push notification travels from our secure servers through the necessary public gateways (like Apple’s Push Notification Service or Google’s Firebase Cloud Messaging) and across the internet to the patient’s phone, the message payload is a garbled, encrypted ciphertext. This prevents any third party—including internet service providers or malicious actors—from intercepting and reading the message content.
- Data at Rest: Encryption isn’t just for moving data. All sensitive information stored within our platform, from patient lists and audience segments to message templates containing PHI, is encrypted at the database level. This ensures that even in the highly unlikely event of a direct breach of our storage systems, the underlying data remains protected and useless to intruders.
By enforcing E2EE by default, we eliminate the risk of human error where an employee might forget to enable a security setting. With indigitall, your patient communications are secured automatically, every time.
Secure, Controlled Infrastructure
A secure message is only as safe as the environment where it is created, stored, and managed. The indigitall platform is hosted within a fortified digital infrastructure that is designed to meet and exceed the stringent Physical and Technical Safeguards outlined by the HIPAA Security Rule. We partner with top-tier cloud providers to host our services in data centers that are themselves compliant with the highest industry standards, such as SOC 2 Type II and ISO 27001.
Our commitment to a secure infrastructure includes:
- Physical Security: Our data centers feature multi-layered security controls, including 24/7/365 monitoring, biometric access screening, and redundant systems for power and cooling to ensure constant operational integrity.
- Network Security: We deploy advanced firewalls, intrusion detection and prevention systems (IDPS), and robust network segmentation to shield our platform from external threats and prevent unauthorized lateral movement within our environment.
- Proactive Threat Management: Our security posture is not static. We conduct regular, rigorous vulnerability scans, third-party penetration tests, and continuous monitoring to identify and remediate potential threats before they can be exploited.
This comprehensive approach ensures that from the physical server racks to the virtual network configurations, every layer of our infrastructure is hardened against unauthorized access, providing a secure foundation for your patient engagement activities.
Robust Access Controls and Audit Trails
A significant portion of data breaches originate from internal sources, whether through malicious intent or simple human error. The HIPAA Administrative Safeguards require strict controls over who can access ePHI, and indigitall provides the granular tools needed to enforce these policies effectively. Our platform features sophisticated Role-Based Access Control (RBAC), allowing you to implement the “principle of least privilege.”
This means you can create custom user roles with specific permissions tailored to job functions. For example, a system administrator can grant a clinic manager the ability to send appointment reminders only to patients within their specific department, while a member of the central marketing team can be given permission to send general wellness tips to all patients without having access to any underlying PHI. This granular control dramatically reduces the risk of unauthorized data exposure.
Furthermore, to ensure full accountability, the indigitall platform helps you maintain detailed and immutable audit trails. Helping you keep a digital ledger that tracks every significant action taken within your account, logging crucial information such as:
- User ID and IP address
- Timestamp of the action
- Specific action performed (e.g., user login, campaign creation, message sent)
- The audience segment targeted
These logs are indispensable. They allow you to proactively monitor for suspicious activity and, in the event of an incident, provide a precise forensic record to investigate what happened, determine the scope of a potential breach, and demonstrate due diligence to HIPAA auditors.
The indigitall Advantage: Beyond Technical Safeguards
A truly HIPAA-compliant communication strategy extends far beyond the technical architecture of a platform. While robust encryption and secure infrastructure are the non-negotiable foundations, they are only part of the equation. True compliance involves a dedicated partnership, a deep understanding of legal responsibilities, and the practical tools to manage the most important relationship of all—the one you have with your patients. At indigitall, we deliver this complete compliance ecosystem, providing the legal assurances and the user-management functionalities that turn a secure platform into a trusted extension of your healthcare services.
Your Partner in Compliance: The Business Associate Agreement (BAA)
Under HIPAA, any vendor that creates, receives, maintains, or transmits Protected Health Information (PHI) on behalf of a healthcare provider (a “Covered Entity”) is considered a “Business Associate.” The law is crystal clear: a formal, signed contract known as a Business Associate Agreement (BAA) must be in place between these two parties. This BAA is not a mere formality; it is a legally binding document that obligates the vendor to uphold the same stringent privacy and security standards as the provider.
Many technology companies, particularly those who do not specialize in the healthcare sector, are often unwilling or unable to sign a BAA. This is the ultimate red flag, as it indicates they are not prepared to accept the legal liability that comes with handling sensitive patient data. Partnering with a vendor without a BAA in place is a direct HIPAA violation, and it leaves the healthcare provider solely responsible for any breach caused by their vendor’s negligence.
At indigitall, we eliminate this risk entirely. We readily sign a Business Associate Agreement with every one of our healthcare clients. This is our formal commitment to you and your patients. By signing the BAA, we are not just providing a piece of software; we are entering into a true compliance partnership. We contractually accept our legal and financial responsibility to implement all required HIPAA safeguards and to report any security incidents or breaches promptly. This “shared responsibility model” means you are not navigating the complexities of compliance alone. You have a partner who is equally invested and legally bound to protect the PHI that flows through our systems, giving you the institutional confidence to innovate in your patient communications.
Obtaining and Managing Patient Consent
The HIPAA Privacy Rule is built on the principle of patient autonomy. Before you can send a single push notification containing PHI, you must have the patient’s explicit permission, or “opt-in.” However, gaining consent is more than just displaying a default system prompt. It requires a thoughtful approach that builds trust and clearly communicates value.
Best Practices for Creating Clear Opt-in Prompts:
A compliant and effective opt-in process is transparent and user-friendly. We guide our partners to follow these best practices:
- Be Transparent and Specific: Instead of a generic “Allow notifications?” prompt, clearly state who is asking and why. Explain the types of messages patients can expect to receive, such as appointment reminders, medication alerts, or notifications that lab results are ready.
- Use Plain, Accessible Language: Avoid technical jargon or dense legal phrasing. The request should be easy for anyone to understand.
- Highlight the Value: Briefly explain how these notifications will benefit the patient, such as helping them stay on top of their care schedule or receiving important health information faster.
- Reassure Users of Control: Always let patients know that they are in full control and can easily manage or disable notifications at any time through their device or app settings.
How the indigitall Platform Manages Consent Seamlessly:
Indigitall provides the robust, integrated tools to implement these best practices flawlessly. Our platform automates the complexities of consent management:
- Intelligent Opt-In Triggers: You can configure the native iOS or Android consent prompt to appear at the most opportune moment in the patient journey, such as after they have successfully logged into their patient portal, increasing the likelihood of a positive response.
- Automatic Consent Tracking: Once a patient opts in or out, their status is instantly and automatically captured as a key attribute in their unique user profile within the indigitall dashboard. This creates a reliable, timestamped record of consent for every user.
- Segmentation for Compliance: This consent attribute becomes a powerful tool for ensuring compliance. When building a campaign, you can effortlessly create a target segment that only includes users where “Push Notification Consent = True.” This simple rule prevents messages from ever being sent to unconsented users, virtually eliminating the risk of a privacy violation.
- Effortless Opt-Out Management: Our system is synced with the device’s operating system. If a patient revokes their permission in their phone’s settings, indigitall automatically updates their profile and excludes them from all future push notification campaigns, ensuring their choice is always respected.

Use Cases: How Healthcare Providers Leverage indigitall
A secure, compliant platform is only as valuable as the outcomes it helps you achieve. The true power of indigitall lies in its application—transforming theoretical features into practical solutions that solve everyday challenges for healthcare providers and enhance the patient experience. By leveraging our HIPAA-compliant push notification capabilities, organizations can move from reactive communication to proactive patient engagement. Below are some of the most impactful ways our partners use the indigitall platform to improve efficiency, support patients, and drive better health outcomes.
Appointment Reminders: Reduce No-Shows with Timely, Secure Alerts
The Challenge: Missed appointments are a significant drain on the healthcare system, leading to wasted clinician time, disrupted schedules, and billions in lost revenue annually. Traditional methods like manual phone calls are labor-intensive and inefficient, while email reminders are often lost in cluttered inboxes.
The indigitall Solution: Our platform allows you to automate a smart, multi-step reminder sequence that is both effective and secure. Using our segmentation tools, you can send personalized, timely push notifications directly to a patient’s mobile device. Imagine a patient receiving an initial alert 72 hours before their visit with an easy option to confirm or reschedule, followed by a final, “just-in-time” reminder 24 hours prior. Each message, such as “Reminder: Your appointment with Dr. Miller at our Raleigh clinic is tomorrow, October 9th, at 11:00 AM,” is fully encrypted and sent only to opted-in users, ensuring complete HIPAA compliance.
The Benefit: This proactive approach drastically reduces patient no-show rates, directly increasing revenue and optimizing your operational workflow. It frees up administrative staff from making hours of manual calls, allowing them to focus on higher-value patient interactions. For patients, it provides a convenient, helpful service that fits seamlessly into their daily lives.
Medication Adherence: Improve Patient Outcomes with Personalized Reminders
The Challenge: Medication non-adherence is a critical public health issue, leading to poor management of chronic diseases, increased hospital readmissions, and preventable deaths. Patients often forget to take their medication or refill prescriptions on time, especially when managing complex treatment regimens.
The indigitall Solution: Indigitall transforms a patient’s smartphone into a supportive health companion. Our platform enables you to create and schedule discreet, personalized medication reminders that are tailored to a patient’s specific needs. For a patient managing diabetes, you could automate daily glucose check reminders. For a post-operative patient, you could schedule a sequence of alerts for their pain management and antibiotic schedule. Messages like “Just a friendly reminder: It’s time for your evening medication,” or “Your prescription is due for a refill in 3 days. Tap here to contact the pharmacy,” are sent securely, providing crucial support between office visits.
The Benefit: This consistent engagement significantly improves medication adherence, leading to better patient health outcomes and a reduction in costly complications and hospitalizations. It empowers patients, making them feel supported and more involved in their own care journey, which strengthens the provider-patient relationship.
Lab and Test Result Notifications: Drive Secure Portal Engagement
The Challenge: Notifying patients that their lab or test results are available presents a classic HIPAA dilemma. You need to inform the patient promptly, but you absolutely cannot disclose the actual results—the PHI—in an insecure message. This often leads to inefficient phone tag and administrative bottlenecks.
The indigitall Solution: A push notification is the perfect tool for this scenario when handled correctly. With indigitall, you can send a secure, encrypted, and generic notification that drives action without disclosing PHI. A simple, compliant message like, “Your recent lab results are now available. For your privacy, please log in to our secure patient portal to view them,” achieves the goal perfectly. This not only informs the patient instantly but also serves as a powerful driver for patient portal adoption and usage.
The Benefit: This process eliminates administrative delays and reduces the burden on your staff. It provides patients with immediate notification and a clear, secure path to their health information, increasing their engagement with your digital health tools and EMR portal.
Telehealth Communication: Facilitate Seamless Virtual Care
The Challenge: The rise of telehealth has introduced new logistical hurdles. Ensuring patients have the right link, remember to join their virtual visit on time, and know the next steps after the call requires clear, timely communication.
The indigitall Solution: Our platform acts as the communication backbone for your virtual care services. You can automate push notifications to be sent 15 minutes before a telehealth appointment, including a secure deep link that takes the patient directly into the video conference with a single tap. Following the visit, another automated push can guide them to their after-visit summary, new prescriptions, or a link to schedule a follow-up. Example messages include “Your telehealth visit with Dr. Garcia is starting soon. Click here to join now,” or “A summary of your recent virtual visit is now available in your portal.”
The Benefit: This streamlined communication drastically reduces late arrivals and technical difficulties for telehealth appointments, creating a smoother, more professional experience for both patient and provider. It ensures better continuity of care by closing the loop after the visit, making sure patients receive and act upon crucial follow-up instructions.
Choosing indigitall as Your HIPAA Compliant Partner
Selecting a communication vendor is one of the most critical decisions a healthcare organization can make. Your partner is not just a software provider; they are a steward of your patients’ most sensitive data and a key factor in your overall compliance posture. As you evaluate your options, it’s essential to move beyond surface-level features and ask the tough questions that separate truly compliant platforms from the rest.
A Checklist for Vendor Selection
Use this essential checklist to vet any potential communication partner. A failure to answer “yes” to any of these questions should be a significant cause for concern.
- Does the vendor readily sign a Business Associate Agreement (BAA)? This is the most critical question. A BAA is a non-negotiable legal requirement under HIPAA that contractually obligates the vendor to protect PHI. Yes, indigitall readily signs a BAA with all healthcare clients, formally accepting our shared responsibility in your compliance journey.
- Is all patient data encrypted end-to-end (E2EE)? Your vendor must be able to protect data both as it travels across networks (in transit) and while it is stored on their servers (at rest). Yes, with indigitall, state-of-the-art E2EE is the default standard, ensuring your messages are unreadable to any unauthorized party at every stage.
- Can you control user access and view detailed audit logs? Internal governance is just as important as external security. You need granular control over which staff members can access and send patient communications. Yes, our advanced dashboard features robust Role-Based Access Controls (RBAC) and immutable audit trails, giving you full control and transparency over all platform activity.
The Power of an Omnichannel Platform
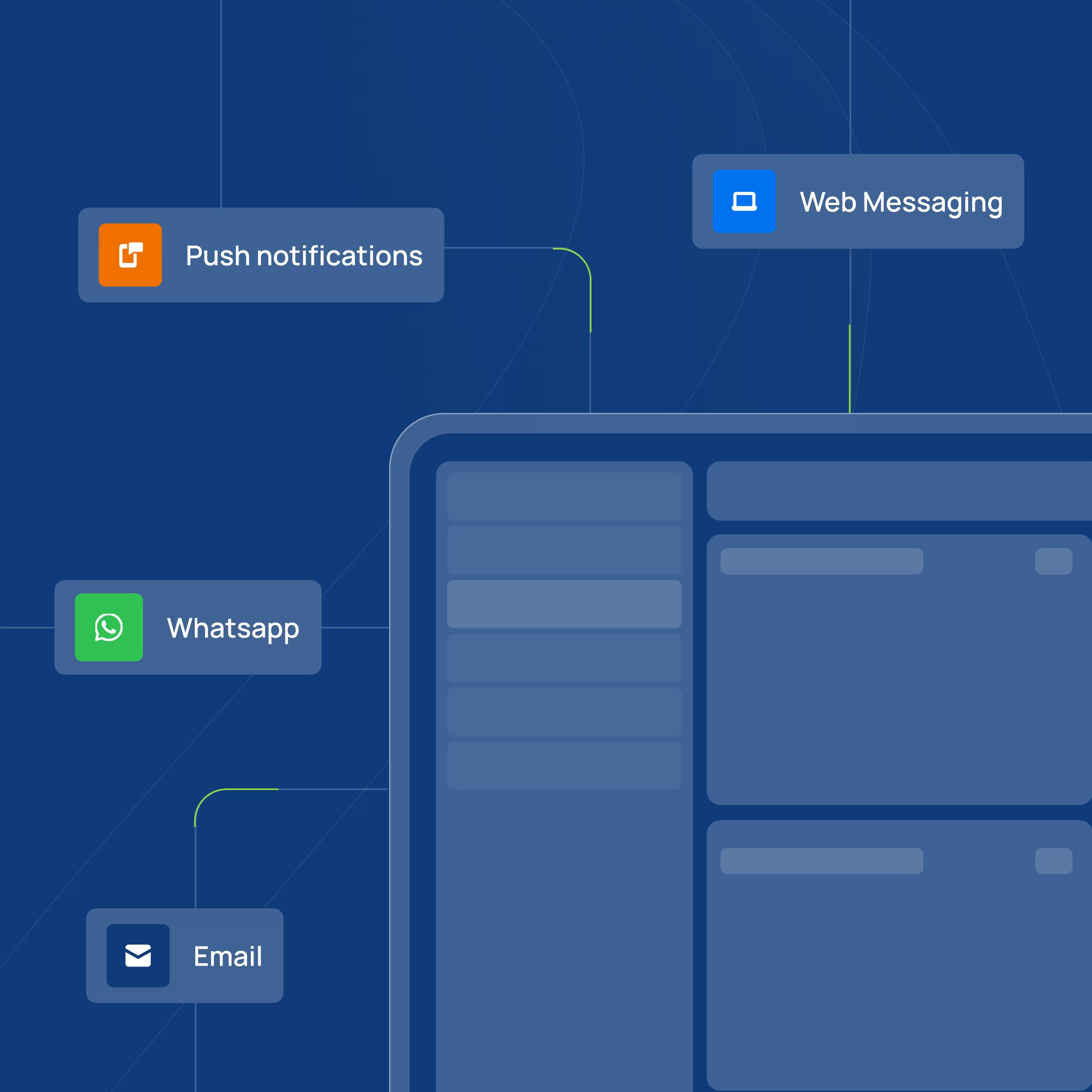
While this guide has focused on the power and complexity of push notifications, modern patient engagement is not limited to a single channel. A truly effective communication strategy meets patients where they are, using the right channel at the right time. This is the core advantage of indigitall’s omnichannel platform.
Beyond push notifications, indigitall allows you to create cohesive, secure patient journeys using a full suite of integrated channels, all managed from a single, unified dashboard:
- SMS: For critical, time-sensitive alerts that need to reach patients who may not have your app installed or notifications enabled.
- In-App Messages: For rich, contextual communication with patients who are actively using your mobile application, ideal for delivering educational content or detailed instructions.
- Web Push: To engage patients through their desktop or mobile web browser, providing a consistent experience even without a dedicated mobile app.
Most importantly, our unwavering commitment to HIPAA compliance applies across this entire ecosystem. Whether you are sending a push notification, an SMS, or an in-app message, the same rigorous encryption, security protocols, and administrative safeguards are in place. This allows you to design sophisticated communication workflows—for instance, automatically sending an SMS if a critical push notification is not opened—with the complete confidence that every touchpoint is secure and compliant.
Conclusion: Build Trust and Improve Outcomes with indigitall
In today’s connected world, the demand for instant, digital communication in healthcare will only continue to grow. Leveraging tools like push notifications is no longer an innovation but a necessity for engaging patients, improving health outcomes, and creating operational efficiency. However, as we’ve explored, this power comes with the immense responsibility of protecting patient privacy under HIPAA. Choosing the right technology partner is the single most important decision you will make in navigating this landscape.
For too long, healthcare providers have been forced to believe they must make a choice between meaningful patient engagement and ironclad security. With indigitall, this is a false choice. We built our platform on the principle that the most effective engagement is born from a foundation of absolute trust. You can and must have both.
When your patients know their data is safe, they are more willing to engage, leading to stronger relationships, better adherence, and ultimately, healthier lives.
Ready to see how indigitall can transform your patient communication strategy while upholding the highest standards of HIPAA compliance? Schedule a demo today.